Glaucoma is a disease of the optic nerve caused by eye pressure. The optic nerve becomes damaged and the patient starts to lose peripheral vision. If left untreated total irreversible blindness may occur. Glaucoma is the leading cause of blindness in people over 60 years old. Early detection and treatment may prevent the development of blindness.
Glaucoma
source – American Academy Ophthalmology
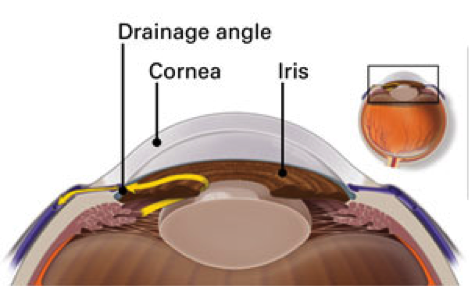
- The eye has a constant circulation of fluid called the aqueous which keeps the eye pressure at a normal level. The aqueous is secreted from a part of the eye called the ciliary body located behind the iris. The aqueous circulates forward and escapes between the iris and the lens into the front chamber of the eye. It drains into a tube running 360 degrees around the eye near the edge of the cornea called the trabecular meshwork and canal of schlemm.
- Glaucoma will develop if there is any imbalance in the aqueous circulation by either poor drainage or blockages in the path of the fluid. This leads to elevated pressure inside the eye.
- The optic nerve is made up of a million tiny nerves fibres. Light is converted into electrical impulses in the nerve cells of the retina. These impulses are carried away via the optic nerve back to the back part of the brain called the occipital lobe. Here, electrical impulses are perceived as an image. So the optic nerve works like a cable connecting your camera to your TV or computer; without it you cannot generate any images.
- The optic nerve fibres are sensitive to eye pressure. So if the pressure becomes elevated, some nerves inside the optic nerve will start to die and stop working properly. This leads to loss of signals from the retina. Usually the first fibres to be damaged are those dealing with peripheral vision which we use in the dark adapted eye such as for navigational night vision.
- The optic nerve stump seen inside the eye is called the optic disc. Normally we have a small excavation in the optic disc called the disc cup which is about 50% of the disc surface area. In glaucoma, the disc cup enlarges as the nerve fibres die.
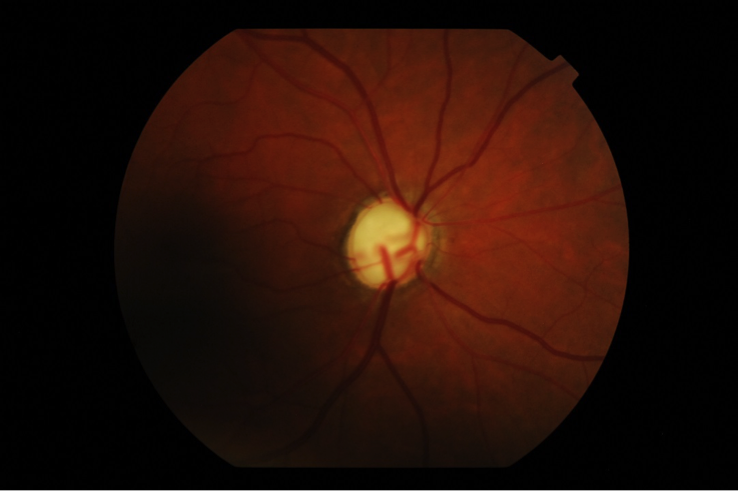
Glaucoma disc cup
Glaucoma can be primary, meaning there is no other underlying cause or secondary, meaning another disease is the reason for subsequent development of glaucoma.
There are two types of Primary Glaucoma:
- Open Angle Glaucoma:
This is the most common type of glaucoma where there is poor drainage of the aqueous fluid in the front part of the eye. This leads to building pressure inside the eye and subsequent damage to the optic nerve. The condition is painless and takes many years to evolve but leads to permanent loss of vision if not treated. This is the most common type of glaucoma in Australia.
- Narrow or closed angle glaucoma
If the front chamber of the eye is shallow, the iris base blocks the drainage angle and prevents fluid easily reaching the drainage tube. This leads to eye pressure build up which eventually damages the optic nerve.
This condition can present as an attack of acute angle closure glaucoma with sudden complaint of seeing haloes around light, blurred vision or severe eye pain. Vomiting can also occur if the eye pressure becomes very high. Immediate treatment is required to abort this attack of glaucoma by undergoing medical and eye laser treatment to open a hole in the iris allowing the aqueous fluid to escape (laser iridotomy). Our centre is equipped with a laser machine to perform this treatment promptly.
In many patients the condition develops slowly (chronic narrow angle glaucoma) with no pain but with ultimate damage to the optic nerve.
- Secondary Glaucoma
There are many causes of high eye pressure secondary to other conditions such as: pseudo exfoliation, pigment dispersion, viral or bacterial infection, inflammatory eye disease or genetic conditions.
- No symptoms: Silent loss of vision
In many cases there are no symptoms until the later stages when patients will notice difficulty with peripheral or night vision. In late stages partial or total irreversible blindness may occur. - Pain, haloes, headaches: in an acute attack of closed angle glaucoma
source – American Academy Ophthalmology
- Over 40 years old
- Family history of glaucoma
- Race: such as of African and Hispanic heritage
- Myopia ( short- sightedness)
- Diabetes, migraine, poor peripheral circulation.
- Eye examination:
- Eye pressure check
- Optic nerve examination
- Anterior chamber and angle examination (gonioscopy)
- Cornea thickness measurement
- Disc photos: to document the optic nerve appearance and degree of disc cupping at initial diagnosis and to monitor it during follow up.
- Visual field testing: to assess the presence of any vision loss and monitor any sign of disease progression.
- Optical Coherence Tomography (OCT): to measure the thickness of the retina nerve fibre layer around the optic nerve.
It is important to realise that treatment does not regain any already lost vision but rather is to prevent further visual loss and blindness.
The aim of treatment is to lower the eye pressure which can be achieved by different methods:
- Eye drops: drops work by either lowering the secretion of aqueous fluid from the ciliary body or by improving the drainage. They need to be used frequently, once or twice every day.
Compliance in using the eye drops is crucial to keep the eye pressure low and prevent further vision loss.
- Laser: is effective in reducing the eye pressure. There are different types of laser that can be applied to different locations;
- Selective Laser Trabeculopalsty: this is used in open angle glaucoma. The laser is very fast and does not cause any coagulation like thermal laser, instead it stimulates the cells in the trabecular meshwork (mesh in front of the drainage tube) to open its pores and increase passage of fluid through them, thus lowering the eye pressure. The procedure is painless and is applied in 2 sessions to the 360 degrees of the drainage tube. It can also be repeated years later without any harm.
- Iridotomy: this is used in cases with narrow or closed angle glaucoma. The laser is used to create a small hole in the iris to allow the trapped fluid behind the iris to escape to the front chamber of the eye, thus relieving the blockage.
- Surgery:
- Trabeculectomy: This procedure is done when open angle glaucoma is not controlled well and the eye pressure remains elevated despite using eye drops and laser. A drainage flap is made in the sclera (white of the eye) to allow aqueous fluid to drain under the conjunctiva creating a bleb under the upper eye lid. This surgery requires regular follow up initially and can be supplemented with certain eye injections to prevent scarring.
- Minimally Invasive Glaucoma Surgery: This procedure has only recently become available and involves placing a micro stent into the trabecular meshwork, or drainage channel of the eye. It is typically performed at the end of Cataract surgery and allows an increased outflow of fluid to reduce the pressure in the eye. It works best for patients with mild to moderate Glaucoma and can result in a reduction in the need for drops.
Want to schedule an appointment?
Call us at (+61) 3 9459 5133 or fill in the appointment form...
