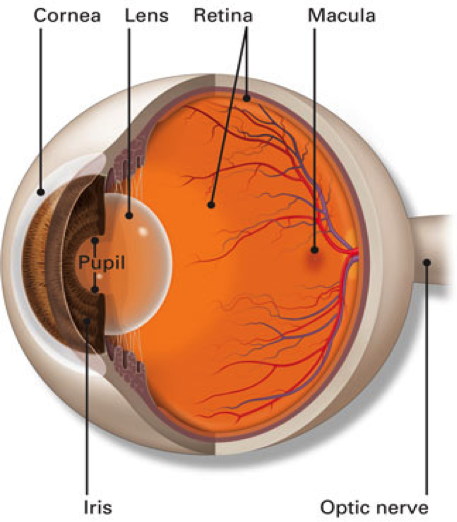
The retina is the inside lining of the back of the eye. It is composed of many layers of light sensitive nerve cells. Light entering the eye is focused on the retina and is converted to electrical impulses which are carried to the brain by the optic nerve. The centre of the retina is called the macula. It is the most sensitive part of the retina and is used for day light and colour vision. This is in contrast to the rest of the retina which is more sensitive in the dark and is mainly used for navigational black and white vision at night.
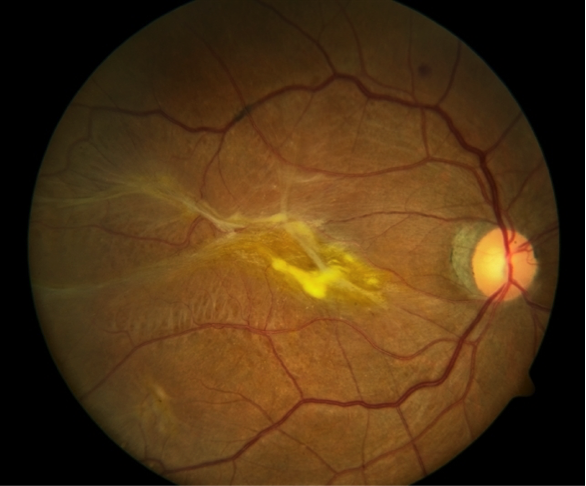
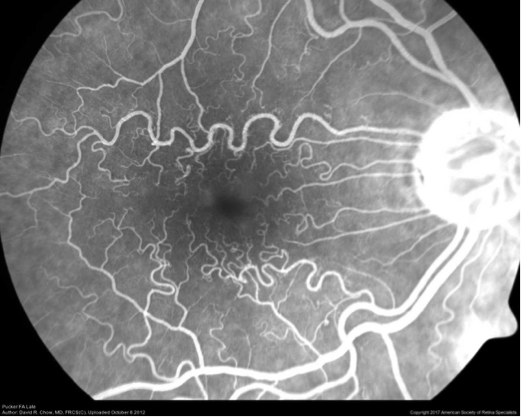
The retina is supplied by one main artery and one main vein which enter through the optic nerve and branch all over the retina to smaller arteries and veins that cross each other’s like railway tracks.