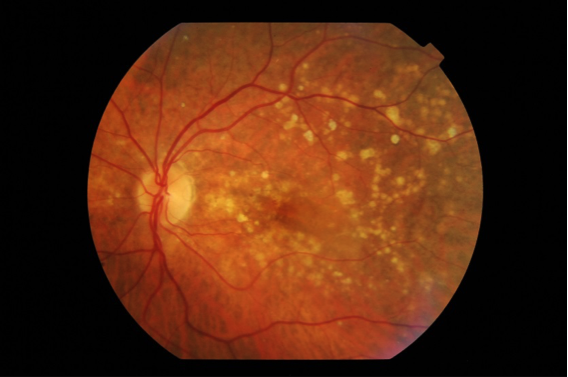
- Treatment of Early Macular Degeneration : Macular Drusen
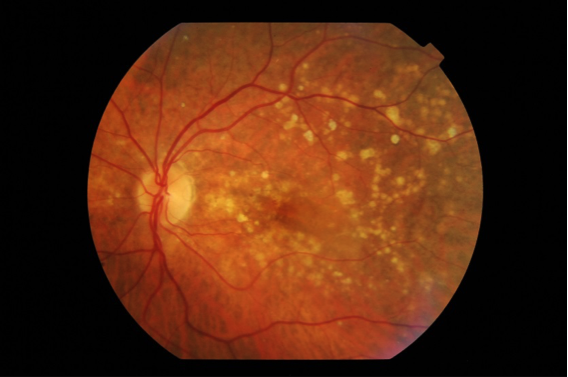
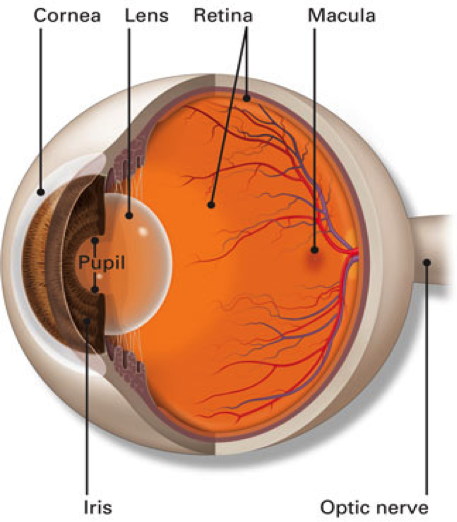
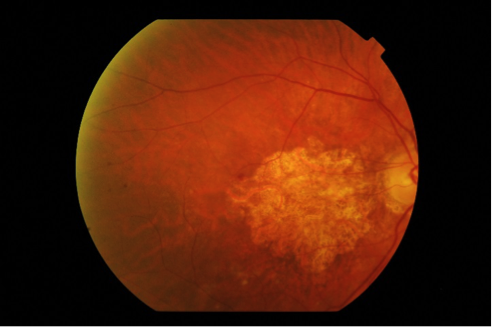
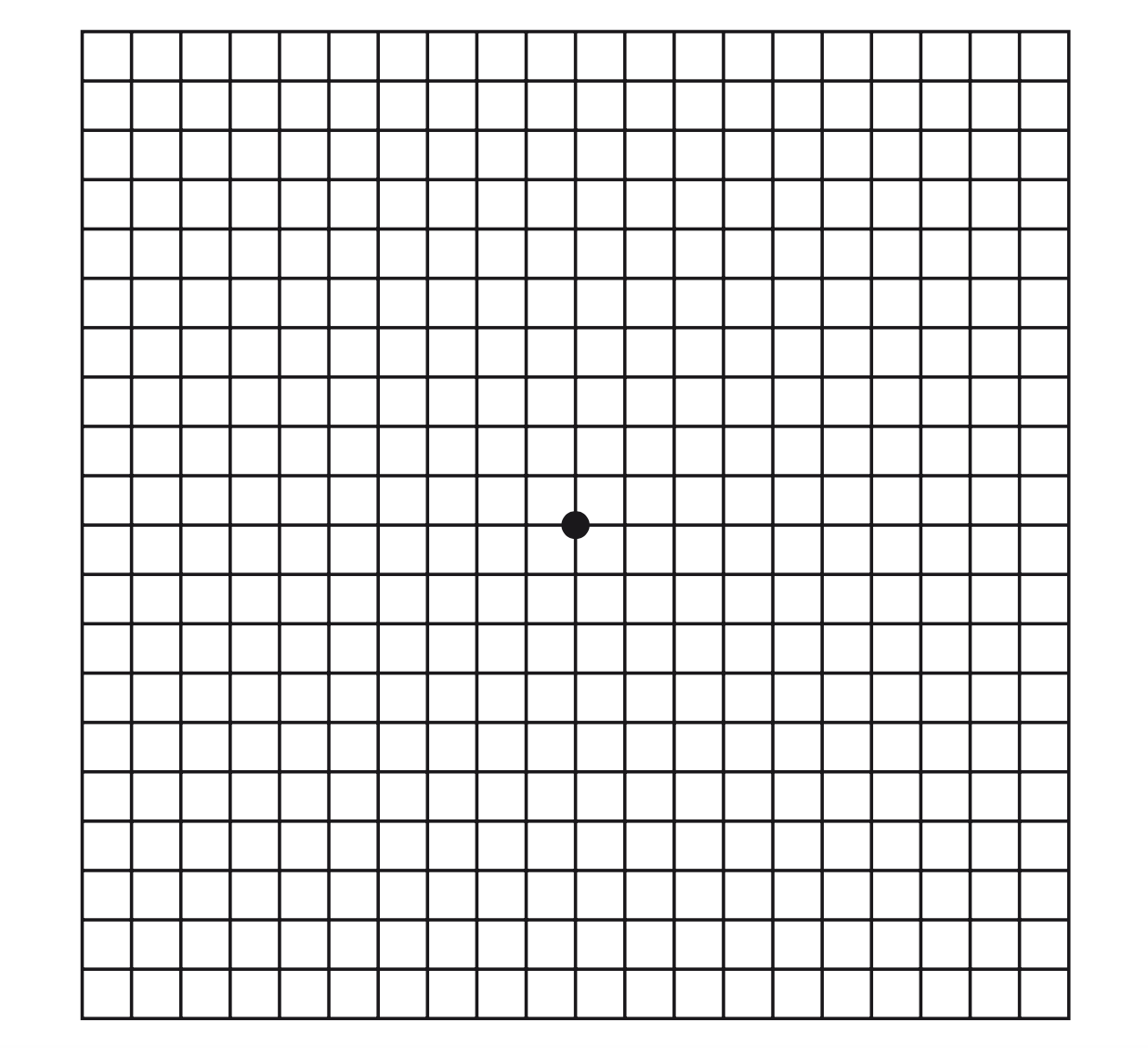
During the early stages of macular degeneration, yellow deposits called “Drusen” appear at the centre of the macula. They usually either give no visual symptoms or cause only slight difficulty with vision. There is no need for intervention at this stage.
- Treatment of Intermediate Macular Degeneration
If the Drusen become large and plentiful, it then indicates some progression and you may be advised to take vitamin supplements.
Antioxidants and Vitamin Tablets
The Age- Related Eye Disease Study 2 (AREDS2)
This large study showed that among people at high risk for developing late-stage, or wet, macular degeneration (such as those who have large amounts of drusen or who have significant vision loss in at least one eye), taking a dietary supplement of vitamin C, vitamin E, lutein and zeaxanthin, along with zinc, lowered the risk of macular degeneration progressing to advanced stages by at least 25 percent. The supplements did not appear to provide a benefit for people with minimal macular degeneration or people without evidence of the disease during the course of the study.
The AREDS2 formula (daily dose) is: Zinc (as zinc oxide) 80 mg, Vitamin C 500 mg, Vitamin E 400 IU, Copper (as cupric oxide) 2 mg, Lutein 10 mg and Zeaxanthin 2 mg
Please note that intake of supplements does not cure macular Degeneration. It only reduces the chance of progression in some cases.
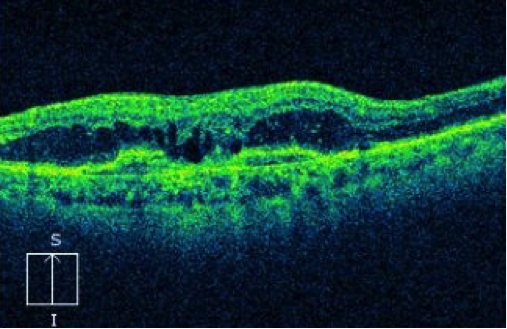
- Treatment of Dry (Atrophic) Macular Degeneration
More common form of macular degeneration and is caused by a breakdown of cells within the macula causing thinning.
Currently there is no proven treatment for dry atrophic macular degeneration, but research is ongoing for new treatment to stop its progression. We anticipate that we will have something to offer our patients with AMD in the next few years. The intake of supplements is advised to reduce the risk of progression.
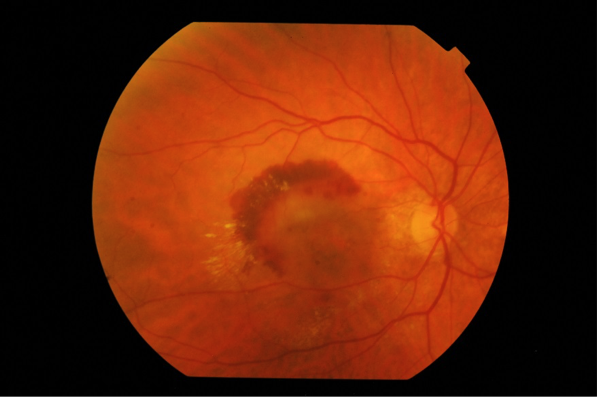
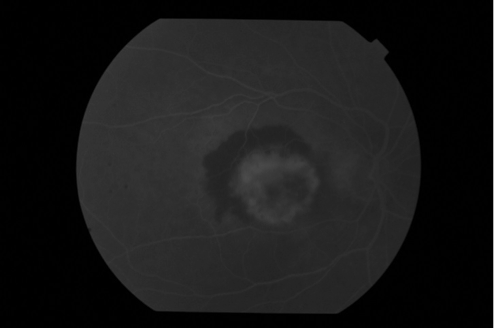
- Treatment of Wet (Neovascular) Macular Degeneration
The most recent and common treatment of wet macular degeneration is injections with drugs called collectively anti-Vascular Endothelial Growth factors (anti-VEGF). Other modalities are also available in certain situations such as laser or photodynamic therapy.
The aim of treatment is to stop the disease and to reduce – but not to eliminate- the risk of severe vision loss. In a considerable percentage of patients vision will improve, especially if they are treated early. However it is important to know that all available treatment does not cure you from the condition.
This is the most common and successful method of treatment of macular degeneration. We have available 3 drugs; Avastin, Lucentis and Eylea. They work in a similar fashion by blocking the effect of chemicals, called VEGF, produced in the eye which cause the new blood vessels to grow under the retina in wet macular degeneration.This will lead the leakage to dry up and stop any bleeding under the macula.
At the Northern Eye Centre, we have special expertise in treating macular degeneration and the centre is organised so that your experience is streamlined with efficiency.
Our treatment rooms are equipped so that you receive the injection whilst you are still comfortably seated in a special chair which is adjusted into position with the least inconvenience to you. The injection is performed under local anaesthesia and only takes minutes to perform.
Anti-VEGF injections need to be repeated every month initially but gradually at longer intervals. If treatment is stopped, the condition becomes active again with loss of initial benefit. It is therefore important that you follow the treatment protocol as advised by our specialist to maintain success and keep your vision sable.
o Laser treatment
In some situations laser treatment may be necessary. Laser is a high energy focused beam of light which causes a small spot of coagulation to the retinal tissue, rather like a localised burn. This will lead to a scarring of the active new blood vessels (neovascular membrane) and stop it from further leakage. Laser is only suitable if the location of this membrane is outside the centre of the macula.
Laser treatment is available at the Northern Eye Centre. It is applied whilst you are sitting in the treatment room, it is painless and takes only a few minutes.
o Photodynamic therapy (PDT)
This treatment involves the combination of cold low- power laser and a light activated drug called photosensitiser. The aim of the laser is to destroy abnormal ‘leaky’ blood vessels.
The procedure is performed at the Northern Eye Centre. It involves injecting the photosensitiser drug slowly into a vein in your arm. The drug will circulate in your body and reaches your retina. The low powered laser beam will then be applied to the location of the abnormal blood vessels under the macula through a special lens. The procedure is completely painless but takes some time to perform.
You will be advised to avoid strong sunlight over the following 3 days. The procedure can be repeated after a few months. PDT is currently only used in a few selected cases and can be combined with anti-VEGF injections.